You might notice shortness of breath, a cough that won’t quit, or wheezing during everyday tasks. COPD is a long-term lung condition that makes breathing harder, but understanding its causes, symptoms, and treatment options can help you take control and feel better. We’ll walk through what COPD is, why it happens, and the choices that can improve day-to-day life.
As we explore signs to watch for, common triggers, and practical treatments from medicines to lifestyle changes, you’ll get clear steps you can use now. Stay with us to learn how to spot problems early, talk with your healthcare team, and make plans that protect your lungs and keep you active.
What Is COPD?
COPD is a long-term lung condition that makes it hard to move air in and out of the lungs. We will explain the main types, how the disease develops, and who faces the highest risk.
Defining COPD and Its Types
COPD stands for chronic obstructive pulmonary disease. It describes lung conditions that block airflow and make breathing harder over time. The two main types are:
- Chronic bronchitis: Long-term cough with mucus. Airways become inflamed and narrowed, which raises the chance of infections.
- Emphysema: Damage to the tiny air sacs (alveoli). The sacs lose their elasticity, so we cannot fully push air out.
Some people have features of both types. Symptoms we often see include frequent cough, sputum (mucus) production, wheeze, and shortness of breath that gets worse with activity. COPD usually gets worse slowly, and changes on breathing tests help confirm the diagnosis.
How COPD Develops
COPD develops when lung tissue or airways are repeatedly injured over many years. The most common cause is cigarette smoking, which damages airways, causes chronic inflammation, and breaks down alveoli. Long-term exposure to air pollution, dust, chemical fumes, or biomass smoke (from cooking or heating) can also cause similar damage.
Repeated infections and a history of asthma can increase the chance of developing COPD. Genetic factors, like alpha-1 antitrypsin deficiency, make some people more vulnerable even if they never smoked. Over time, inflammation and scarring narrow airways and reduce the surface area for gas exchange, which leads to rising breathlessness and lower exercise tolerance.
Who Is at Risk for COPD?
People who smoke or used to smoke have the highest risk. The longer and heavier the smoking history, the greater the risk. We also watch for these risk factors:
- Work exposures: Long jobs with dust, chemical fumes, or vapors.
- Indoor pollution: Regular exposure to biomass smoke from cooking or heating.
- Age: Symptoms often appear in people over 40, but damage can begin earlier.
- Family history: A genetic deficiency (alpha-1 antitrypsin) raises risk even without smoking.
- Past lung infections and childhood asthma:Early lung injury or chronic airway disease increases susceptibility.
We recommend talking to a clinician if you have chronic cough, regular mucus, or increasing breathlessness, especially with these risk factors. A breathing test (spirometry) can confirm whether airflow is limited.
COPD: Causes, Symptoms, and Treatment Options
We explain what commonly causes COPD, how to spot its main symptoms, the treatments doctors use today, and practical steps we can take to live better with the condition.
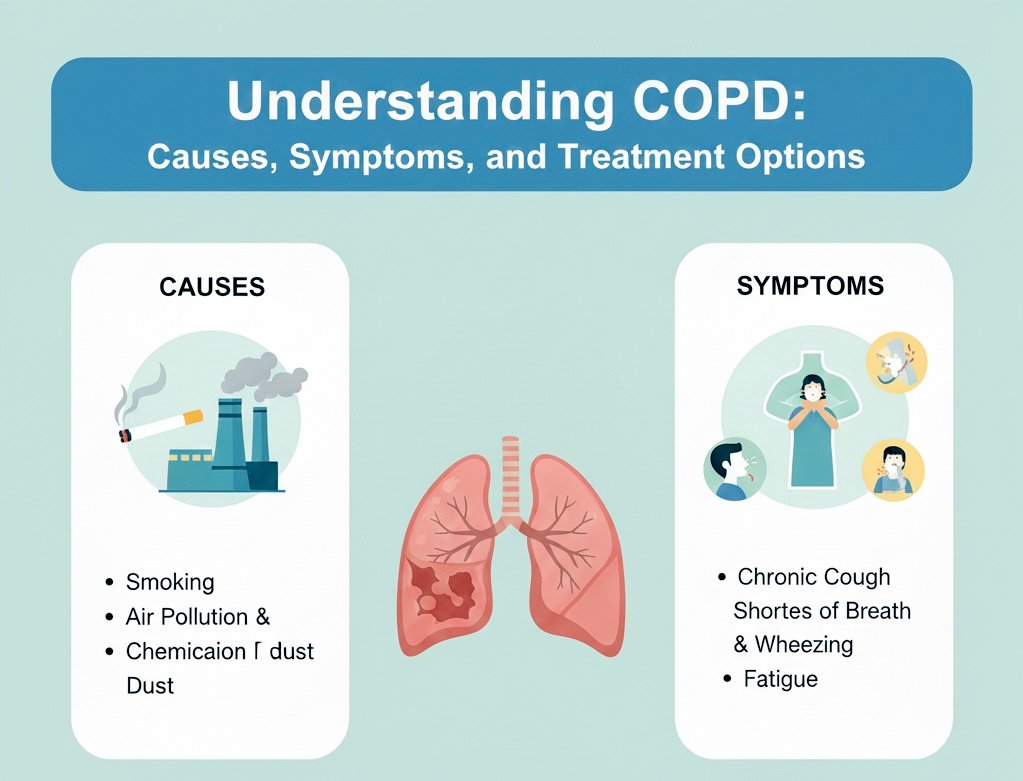
Major Causes of COPD
The top cause of COPD is long-term cigarette smoking. Years of smoking damage the airways and air sacs, leading to chronic bronchitis or emphysema. Secondhand smoke and vaping can also harm lung tissue over time.
Occupational exposures come next. Jobs with dust, chemical fumes, or coal and silica dust raise risk if we lack proper protection. Repeated lung infections and a rare genetic factor called alpha-1 antitrypsin deficiency can cause or worsen COPD in people who never smoked.
Age matters. Symptoms often appear after age 40 because lung damage builds up slowly. Our risk grows if we have a history of asthma that remains uncontrolled into adulthood.
Recognizing Common Symptoms
Shortness of breath during daily tasks is a key symptom. We may notice it first when climbing stairs, walking uphill, or carrying groceries. Wheezing and noisy breathing often come with exertion.
Chronic cough and sputum production are common. A cough that lasts months or returns each year suggests chronic bronchitis. Symptoms can flare during infections; these “exacerbations” may bring worsened breathlessness, increased mucus, and fever.
Fatigue, weight loss, and chest tightness are frequent too. Symptoms can be subtle at first, so we should seek testing—like spirometry—if breathing gets steadily worse or if we have a long smoking history.
Modern Treatment Approaches
Treatment aims to reduce symptoms, prevent flares, and slow decline in lung function. We use inhaled bronchodilators (short-acting and long-acting) to open airways and inhaled corticosteroids for some patients to cut inflammation. Combination inhalers are common.
Pulmonary rehabilitation helps with breathing techniques, exercise training, and education. Oxygen therapy supports people with low blood oxygen. For severe disease, surgical options—lung volume reduction or transplant—may be considered. Vaccines for flu and pneumonia lower infection risk.
Smoking cessation is the single most effective step to slow progression. We pair counseling with nicotine replacement or medications like varenicline when appropriate. Regular follow-up and action plans reduce hospitalizations.
Living Well With COPD
We can improve daily life through exercise and pacing. Low‑impact activities (walking, cycling, light strength training) boost stamina and muscle function. Pulmonary rehab gives structured plans we can follow.
Breathing techniques, such as pursed-lip breathing, reduce breathlessness during exertion. Nutrition matters: maintaining healthy weight and muscle mass helps with energy and breathing effort. Avoiding lung irritants—smoke, strong fumes, and air pollution—limits symptom spikes.
We should create an exacerbation action plan with our clinician. Track symptoms, know when to use rescue inhalers, and seek prompt care for worsening signs. Support groups and counseling help manage emotional stress and keep us motivated.
Conclusion
We learned what COPD is and how it affects breathing. We saw common causes like smoking and lung damage, plus signs such as chronic cough and shortness of breath.
We can take practical steps to manage COPD. Quitting smoking, using prescribed inhalers, and joining pulmonary rehab help reduce symptoms and flare-ups.
We should watch for warning signs of worsening disease. Increased cough, more mucus, or trouble breathing mean we need to contact a healthcare provider right away.
We can support people with COPD by offering practical help. Simple actions — driving to appointments, helping with medications, or encouraging exercise — make daily life easier.
We know research continues to improve care. New treatments and better self-management tools give us reason for cautious hope.
Key takeaways:
- Early diagnosis improves outcomes.
- Lifestyle changes and medications lower risk of exacerbations.
- Support and regular care help maintain quality of life.